As a Registered Nurse and mother, I always knew there was more to the practice of these professions than the rules, science, etc. As I was reading an article today, it really helped me to voice what it takes to be a nurse when addressing one of the most important epidemics of this time – the opioid epidemic.
We all know the statistics of the opioid crisis. We all have a friend, coworker, family member or child who has been affected in some way by this crisis. As nurses, we were taught that pain had become the fifth vital sign, and our role was to eliminate this pain. However, as the article I read questioned: Is it realistic to expect absolutely no pain after surgery or an injury? In nursing school I was taught that increased pain could be a sign of an infection or other complication and that this should be monitored. If we remove all the pain, how do we assess for these complications?
Instead it is more realistic to work towards managing pain. Pain is real, we should always acknowledge and ensure the patient knows we take their pain seriously. A realistic approach to effective pain management is to decrease pain by approximately 50%. At this level one would expect the patient to be able to ambulate, rest, etc.
Nurses are an important part of the team fighting the opioid crisis. As case managers, we have a responsibility to facilitate responsible prescribing and to explore alternatives. We should always request the physician check the Prescription Drug Monitoring Program applicable to the state whenever prescribing controlled prescription drugs. We should be calculating the Morphine Equivalency Dosage of all medications prescribed, with the goal of keeping MED under the CDC recommended levels. Case Managers should be providing education including side effects, proper storage, disposal, and alternate pain relief measures.
Are we calling the injured worker after a controlled prescription drug is prescribed to reinforce teaching to ensure they are taking the medication appropriately, to assess for any side effects, to reinforce non-opioid measures for pain? Are we performing medication reconciliation and sharing the results with the prescribing physician?
In addition to the actions above that are part of the science of nursing are we utilizing the “art” of nursing? Or have we forgotten the art of nursing and are only focused on the science?
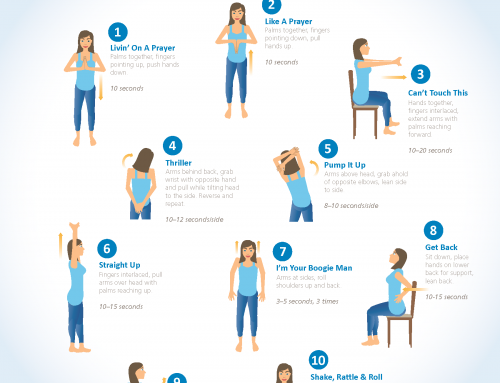
Nursing is both an art and a science and according to the Lippincott Nursing Center, using those principles can help guide our pain management practice through:
- Educating patients that reducing pain, not completely alleviating it, is often the goal.
- Evaluating and managing the patient’s anxiety through relaxation techniques.
- Using correct patient positioning.
- Using ice or heat when appropriate.
- Using compression and elevation for sprains or strains.
- Encouraging rest.
- Using acupuncture, meditation, and other alternative or naturopathic techniques
In my opinion, the healthcare community is always more effective when we combine “art” with science.